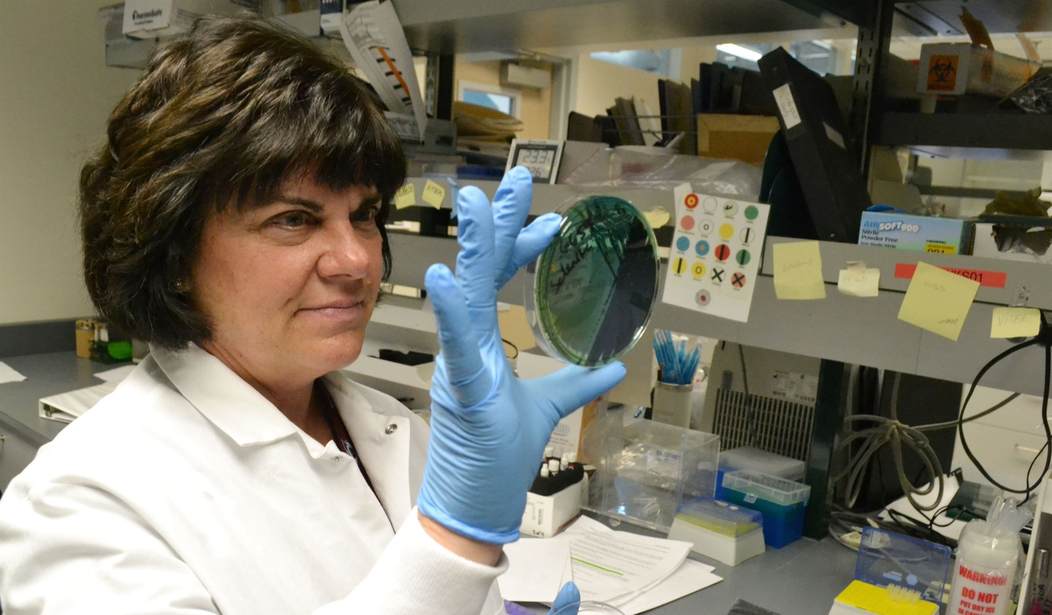
The discovery of penicillin by Alexander Flemming in 1928 was a watershed moment in treating infectious diseases. For nearly a century, the class of drugs the discovery launched, called antibiotics, has saved millions of lives globally. Doctors use these medications to treat bacterial infections, and the World Health Organization lists 81 of them on their list of essential medicines.
While most of the world’s focus has been on viruses since early 2020, bacterial infections cause many illnesses. Viruses or bacteria can cause everything from ear infections to upper respiratory symptoms and sore throats. Antibiotics can often eliminate bacterial infections. They will not kill a virus circulating in the body.
The fun part about bacteria is that some of the ones that commonly cause infection are found on our skin and inside our body as part of our normal flora. Humans routinely have streptococcus and staphylococcus on their skin and mucous membranes. When our immune defenses are down due to fatigue, poor diet, chronic illness, or age, these bacteria can proliferate and cause symptoms. Usually, a course of antibiotics effectively treats these overgrowths.
However, bacteria can mutate just as viruses do. As many people learned during the pandemic, viruses can learn to bypass the defenses of the human immune system. Bacteria can learn to evade the protection provided by an antibiotic. Some antibiotic-resistant bacterial infections you may have heard of are Methicillin-resistant Staphylococcus aureus (MRSA) and drug-resistant Streptococcus pneumonia (DRSP).
According to the Cleveland Clinic, antibiotic resistance (ABR) significantly limits treatment options. ABR is a worldwide health problem, and some strains of bacteria are now referred to as “superbugs.” These bacteria do not respond to several different antibiotics. Cleveland Clinic lists several ways bacteria can become resistant to an antibiotic:
- Overuse of antibiotics: Taking antibiotics when they’re not needed contributes to antibiotic resistance. For instance, viruses cause most sore throats. Antibiotics won’t help.
- Misuse of antibiotics: If a patient forgets to take doses of an antibiotic, stops treatment too soon, or uses an incorrect antibiotic, the bacteria will resume reproducing. As they multiply, they can become increasingly resistant to a specific medicine.
- Agricultural use: Bacteria in animals can also become antibiotic-resistant. An estimated 80% of antibiotic use in the United States is for livestock.
- Spontaneous resistance: The genetic makeup of a bacterium can change or mutate on its own. This change can confuse the antibiotic or help the bacteria fight its effects.
Doctors have used antibiotics broadly for decades, and patients have pushed to get them. School and work policies for returning after an illness encouraged their use. Many require an individual to be fever-free for 24 hours off fever-reducing medication before returning. Antibiotics can hasten this milestone in cases where a patient would recover without them, allowing children to return to school and parents to return to work. Often, patients perceive that antibiotics can’t hurt, even if they don’t help.
However, this is not the case. In addition to contributing to drug resistance, antibiotic use can disrupt the appropriate function of the various bacteria, yeast, and other microbes that perform a role in maintaining human health. Many Americans take prebiotics and probiotics to maintain intestinal health. These preparations are live bacteria that contribute to digestion and immune health.
Related: Here’s to Your Health: Could the Answer to Improving Metabolic Health Be Attached to Your Foot?
Studies show even a required course of antibiotics can disrupt gut health. Infection from the overgrowth of yeast in the body’s normal flora is also common following a course of antibiotics. The duration of the adverse effects depends on the specific antibiotic, the patient’s overall health, and the length of treatment. One study noted that “when many components of the normal flora are eliminated or suppressed by a course of broad-spectrum antibiotics, the stage is set for other organisms that may be pathogenic to step in and cause disease.”
Some patients’ immune systems become overwhelmed when medical providers have difficulty finding an effective antibiotic. This overreaction of the immune response is a condition called septicemia. It can cause multi-organ failure and death. While the CDC estimates that 1.7 million Americans develop these resistant infections and more than a quarter million die because of them, a recent report from Reuters indicates this could be an underestimate:
Fifteen years after the U.S. government declared antibiotic-resistant infections to be a grave threat to public health, a Reuters investigation has found that infection-related deaths are going uncounted, hindering the nation’s ability to fight a scourge that exacts a significant human and financial toll.
Even when recorded, tens of thousands of deaths from drug-resistant infections – as well as many more infections that sicken but don’t kill people – go uncounted because federal and state agencies are doing a poor job of tracking them. The Centers for Disease Control and Prevention (CDC), the go-to national public health monitor, and state health departments lack the political, legal and financial wherewithal to impose rigorous surveillance.
Antibiotics have a place in treating illness, yet they carry risks. Their effectiveness also must be reserved for patients who cannot effectively fight off a bacterial illness on their own. The FDA approved the last new class of antibiotics in 1987, which limits the arsenal of tools doctors can employ.
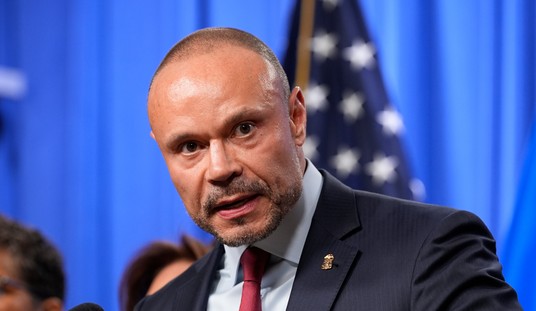
“We believe that through proper education, a lot of antibiotic misuse can be curbed,” said Shawn Rowland M.D., the founder of JASE Medical. His company provides medication supplies, including antibiotics, for people to have on hand in case of an emergency. Rowland believes that providers should use all the tools available through telemedicine to improve patient assessment and education about antibiotics. Questionnaires sent through e-mail and automatic text reminders to take antibiotics as directed are two that are currently available. In his opinion, education to prevent overuse and misuse, not restricted use, is the correct answer.
Recommended: Woke Wednesday: A Whole Generation of Kids Is Being Destroyed by the Left
Cleveland Clinic provides some things everyone can do to prevent antibiotic resistance. People should only take antibiotics prescribed for them. Do not take another person’s antibiotics. They may not be effective for your infection and may not be the correct dose if prescribed by weight. Set reminders on your phone, so you don’t miss a dose of antibiotics, and take the entire prescription even if you feel better. If you forget to take your medicine, ask your provider what to do. The doctor may switch you to a new drug depending on the circumstances.
There are also several things everyone can do to prevent unnecessary use. If you or your family member are otherwise healthy, talk to your healthcare provider about treating and monitoring symptom improvement for a period of time before beginning antibiotics. Your body’s defenses may fight off the illness without an antibiotic. Also, insist on an appropriate test to determine if bacteria and not a virus are causing your symptoms before taking an antibiotic.
Finally, take all of the measures you can to prevent getting sick. Wash your hands regularly. Good hygiene lowers your risk of getting a bacterial infection. Teach children not to share straws, cups, and other utensils. Get regular exercise and eat a healthy diet that includes meat and dairy produced without antibiotics. Get about 20 minutes a day of sun exposure if you can, and talk to your doctor about vitamin D supplementation if you can’t.
You are fearfully and wonderfully made. Partner with your healthcare professional and use antibiotics correctly to preserve their effectiveness for the future.








Join the conversation as a VIP Member