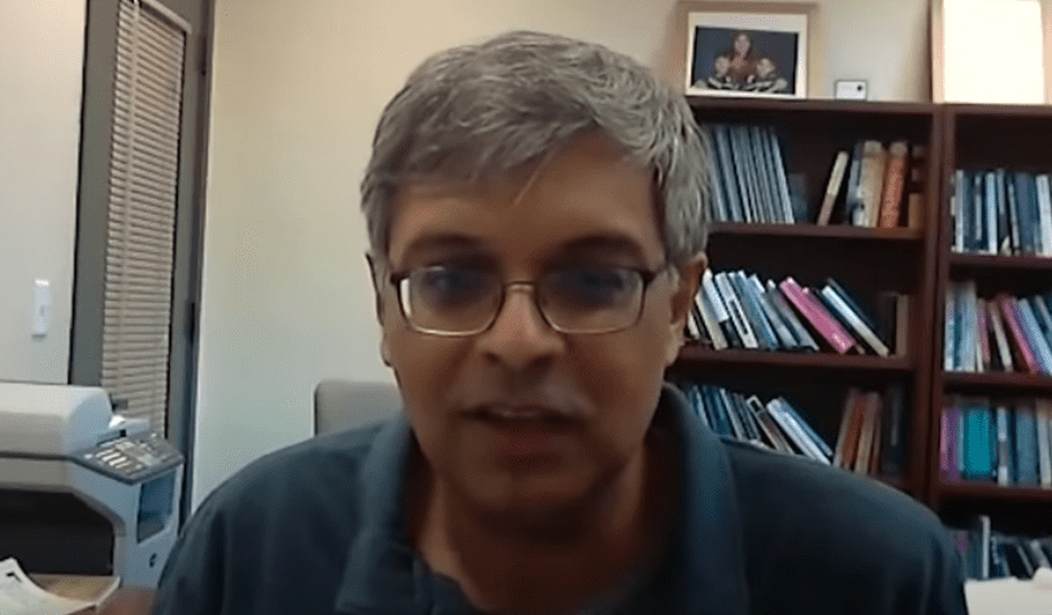
Dr. Jay Bhattacharya of Stanford Medicine recently released his antibody study of the staff of 27 Major League Baseball (MLB) teams from across the nation. The study is of mostly staff, not players, and covered a broad demographic range. The results of the MLB study showed that only 0.7% of the staff had the antibodies indicative of having had COVID-19.
Some staff is located in areas where antibody testing has been conducted for the general population such as New York, Los Angeles, and Santa Clara. Most of these locations showed the MLB staff had a much lower rate of prior infection than the general population. For example, the New York City metro area showed 25% of the population had antibodies. The MLB staff for the Yankees only showed antibodies in 1.64% of the employees. The Mets tested positive at a rate of 2.61%.
Dr. Bhattacharya said this was indicative of a trend seen in the other studies he has done. Lower-income residents had higher exposure rates to COVID-19. While the MLB had put mitigation policies in place, he believes that middle-to-upper-income individuals, like most of these staff in this study, have lower exposure. The ability to work from home and live in areas away from where they work that are less densely populated may be a factor.
The conclusion that Dr. Bhattacharya comes to based on the studies he has done to date is that the epidemic is far from over. The good news is his studies show about 70% of those who display antibodies were asymptomatic. This testing also places the death rate at somewhere between 0.1- 0.5%. This is orders of magnitude lower than originally thought.
This is important because, according to Dr. Bhattacharya, containment strategies are not likely to be effective and the virus is not going to disappear:
“I think in the back of people’s heads there is this idea that somehow we can eradicate this disease if we just stay locked down. That is not possible. The serologic evidence, even the MLB study, suggest this. It suggests the epidemic is too widespread to eradicate. It spreads via asymptomatic contact. Like people who don’t have very many symptoms, even mild cold symptoms can spread the thing. They aren’t going to show up for testing. They aren’t going to show up at a hospital or a doctor.”
He said containment could actually backfire if a positive test requires forcible quarantine of the individuals and members of their households as some public officials are proposing. In these circumstances, he said people may begin to avoid testing. Then he added that lifting lockdowns will absolutely cause an increase in the spread of the illness. Lockdowns have simply delayed the full spread.
Dr. Bhattacharya is clear:
“There is no safe option. If you think that having a lockdown will provide you safety, you are mistaken. Because the problem is this lockdown has had enormous negative effects on the health of people in the United States and around the world.
For example, 1.4 million tuberculosis patients in India are not getting critical antibiotic treatments due to shutdowns. In the U.S., we know chemotherapy patients have missed treatments. Individuals have suffered heart attacks and strokes at home rather than go to the hospital, and mental health resources have seen staggering increases in calls. He also referenced the lagging deaths of despair that are likely, saying the current impacts will be larger than the 2008 recession.
Based on his research to date, Dr. Bhattacharya advocates for lifting lockdowns based on local experience data. His sense, though he has not confirmed via testing, is that this could be accomplished in most areas of the country. He also has some ideas of what the priorities need to be in proceeding, including widespread disease testing. He agreed with Dr. Fauci’s previous statement that disease testing is simply an answer at a point in time. A negative test does not confer any long-term assurance.
When asked, Dr. Bhattacharya clearly understood the political calculations that leaders are making. He said leadership is what is needed because politicians are going to face the consequences of COVID-19 or the problems caused by economic collapse. According to his assessment, a vaccine is an open-ended question. None of the other coronaviruses that infect humans have one and there is no guarantee this one will. So, he recommended the following:
- Protect at-risk groups that are obvious such as nursing home residents. The disease most often seems to require some extended close contact to spread, so these environments need to be addressed.
- Continue to share clinical information broadly. Ventilator protocols have improved significantly based on the sharing of best practices. This will result in more effective treatment.
- Use the current global clinical information to determine more precisely who is at risk for severe illness with a COVID-19 infection.
He said the final bullet should be the focus for epidemiologists. For example, we know the elderly have a higher risk. But not all elderly patients suffer from severe disease. For those who suffered severe disease or death below the age of 65, what were their common health, demographic or genetic profiles? If researchers could refine this picture, then individuals and public health services could be advised appropriately.
Here is the full interview with Dr. Bhattacharya and Peter Robinson of the Hoover Institution. It is a balanced and data-driven assessment that is sorely needed.
Editor’s Note: Want to support PJ Media so we can keep telling the truth about China and the virus they unleashed on the world? Join PJ Media VIP and use the promo code WUHAN to get 25% off your VIP membership.








Join the conversation as a VIP Member