On March 5, 2021, the CDC issued a study that they conclude should recommend mask mandates nationwide and closure of indoor spaces such as restaurants and bars. As with all studies, the devil is in the details. For a health bureaucracy that harps on the need for random, controlled, double-blind studies, the recommendations based on this one are alarming. The Netherlands did the only recent analysis using that gold standard to assess the effectiveness of mask-wearing to prevent the transmission of COVID-19. It showed no statistically significant difference between people who wore masks and those who did not in contracting COVID-19.
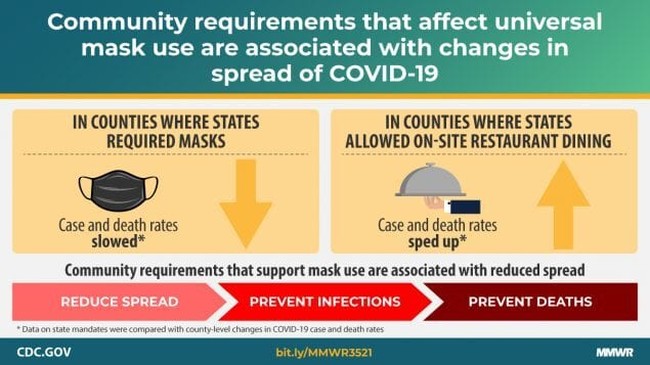
Still based on the new analysis, the CDC produced this graphic:
Is that technically what they found? Sure. The problem is with how they found it. In the study, they use mask mandates by county as a proxy for the behavior of mask-wearing. This assertion is a gross over-assumption given polls regarding the use of masks nationwide. For example, one poll in October showed adults (93%) said they sometimes, often or always wore a mask or face covering when they leave their home and are unable to socially distance, including more than seven in 10 (72%) who said they always did.
Mask wearing varied based on age, gender, and political affiliation, but it found that all of these groups increased their mask use beginning in the fall when cases began to rise. People who reported mask-wearing “sometimes” or “often” likely did so in the environments where they were required or indoors, where social distancing is not possible and where transmission is most likely. Even the CDC does not list outdoor transmission as a common vector. Instead, it depends on the closeness of contact and duration.
Additionally, the study does not account for individual businesses, schools, and other establishments requiring the use of masks even when the government did not. So, while they found differences, it is impossible to link them to a government mandate given the individual variation in mask-wearing with increased compliance over time and variation in the community among businesses and other indoor spaces requiring masks.
Even with those caveats, the differences they found were minimal. Regarding mask mandates:
- Mask mandates were associated with a 0.5 percentage point decrease (p = 0.02) in daily COVID-19 case growth rates 1–20 days after implementation.
- Decreases of 1.1, 1.5, 1.7, and 1.8 percentage points 21–40, 41–60, 61–80, and 81–100 days, respectively, after implementation.
While the study has an appropriate p-value to indicate statistical significance, the underlying assumptions are wrong about mask-wearing in the population. A Lancet study that included almost 400,000 individuals contradicts the assumption in the CDC study:
Self-reported mask-wearing increased separately from government mask mandates, suggesting that supplemental public health interventions are needed to maximise adoption and help to curb the ongoing epidemic.
So, more people were wearing masks whether the government told them to or not. One might deduce that people can make good decisions in light of the circumstances in their community and assess their risk. It may shock our leadership class, but Americans are relatively bright.
In an astounding second conclusion, the study links indoor dining to death rates. The findings contradict previous studies that show low rates of transmission in restaurants and bars. The public slammed local leaders in Nashville for not disclosing this type of data in a city that relies on income from these establishments. Only 80 cases had been linked to establishments on Broadway downtown as of September. Construction sites and nursing homes accounted for more than 1,000 cases each. However, local leaders only targeted restaurants and bars for restrictions at the time.
In New York City, 1.3% of cases came from restaurants. The CDC reported that outpatients who were in a restaurant in the last 14 days were twice as likely to have a positive COVID-19 test. However, it did not distinguish between indoor and outdoor dining, measure for confounding variables during the 14 days, or exclude the 42% who said they were in close contact with an infected patient. Then there is the genuinely stunning admission in the study about testing:
Finally, case or control status might be subject to misclassification because of imperfect sensitivity or specificity of PCR-based testing.
So, even people with a positive test may not have had COVID-19 because the PCR test is not reliable. Continuing to use these tests to make such drastic public policy decisions understanding their flaws, is astounding.
The overstatement of the case in the latest CDC study is astounding as more and more Americans are vaccinated, and a significant portion of the population has likely been exposed. It can be assumed both of these groups have some level of effective natural immunity. Additionally, many areas of the country are heading into better weather, and the effects of temperature and humidity on the virus were documented last year. A cynical person may think our political class is invested in supporting the lockdown bros in limiting Americans’ ability to make a living and gather together forever.










