Despite the ubiquitous presence of Dr. Anthony Fauci on television to pontificate about COVID-19, it appears the National Institutes of Health (NIH) spent very little of its expansive budget on COVID research. In an analysis in preprint, researchers found only 2% of the NIH budget was allocated to COVID studies early in the pandemic. The investigation found that 2% of grants and 5.3% of the NIH budget got allocated to COVID research in 2020 overall. It also found that the average time to award a grant was 151 days.
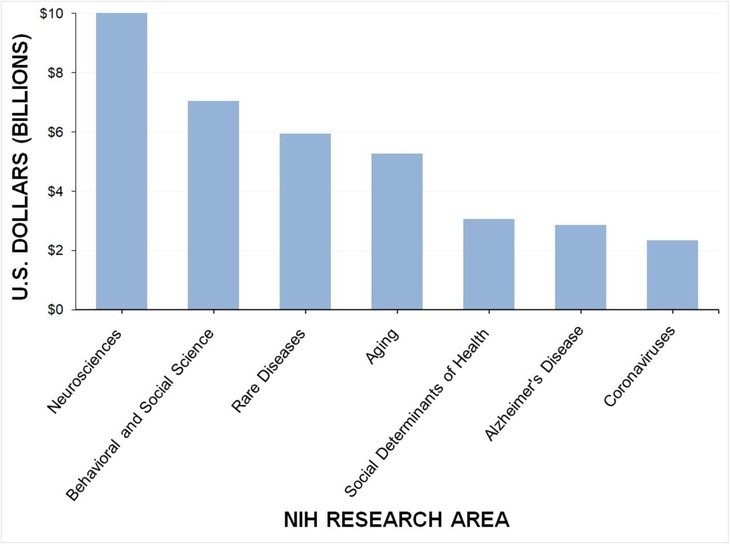
This graph shows where COVID research funding ranked in 2020, while children were out of school, businesses stayed shuttered, and Americans were dying:
The stated mission of the NIH is to undertake research and apply the knowledge gained to enhance health, lengthen life, and reduce illness and disability. By all available evidence, the COVID pandemic was the most urgent health crisis in a century and cut the lives of nearly one million Americans short. After two years, there are still limited outpatient treatments available. In-hospital treatment protocols still rely almost exclusively on remdesivir, a drug the World Health Organization recommended against in November of 2020.
COVID-19 systemic inflammation begins in the lungs and produces overwhelming clotting that kills people suffering from severe infection. Yet health system administrators and politicians still prohibit doctors from using existing medications to reduce viral replication, relieve respiratory inflammation, and prevent the blood clots. These rules exist because of statements from our public health bureaucracy, including Dr. Fauci and the NIH. Meanwhile, physicians prescribe those existing drugs for any other illness with those symptoms. Just not COVID.
According to the analysis, 85 grants focused on developing new therapeutics (6.4% of COVID funding) and 79 grants focused on existing therapeutics (28.2% of COVID funding). The only therapeutics used before COVID on the NIH treatment protocols are dexamethasone and other corticosteroids. If Sen. Ron Johnson ever gets to launch the investigation into the COVID response that he so clearly wants to do, it would be great to audit the nearly 30% of the 2020 COVID spending that looked at existing drugs. Someone with a background in clinical trials and study design should be on that team.
The primary focus of Dr. Anthony Fauci and the NIH was COVID vaccine development. According to the research, 69 grants were awarded for vaccine development (32.2% of COVID funding). Pharmaceutical companies also provided clinical trial funding. Guaranteed purchases by the government ensured Big Pharma would recover the research and development costs if the vaccine earned approval for use.
Dr. Fauci and the NIH used the same strategy of prioritizing a vaccine during the HIV epidemic. There is still no vaccine to protect against HIV, and to date, we have two versions of what they call a vaccine for COVID. The CDC had to change the definition of the word vaccine to make these therapeutics fit. Not even a year after initial doses, the CDC recommends “boosters.”
Recommended: The CDC Data Nobody Is Talking About Raises Urgent Questions for Bureaucrats
The CDC just announced that the booster of the mRNA shot is effective for around four months. It appears these vaccines will be something akin to the Columbia House Record Club. Those of us who are above a certain age would understand that this means you get a vaccine, whether you want it or not, every few months. According to the latest study:
Researchers found the booster shots remained highly effective against moderate and severe covid-19 for about two months after a third dose. But their effectiveness declined substantially after four months, suggesting the need for additional boosters, the study said.
The review shows that the largest amount of COVID funding went to infrastructure and education research in 2020. The study authors noted:
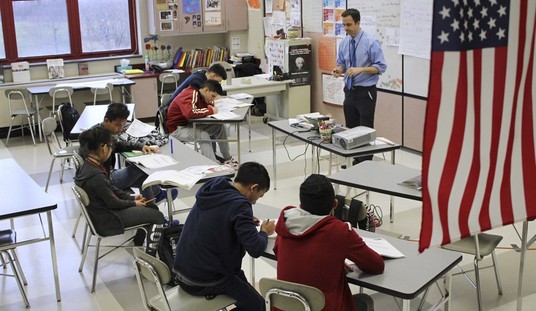
Infrastructure and education accounted for 55.9% of NIH COVID-19 funding, yet many of the major clinical questions surrounding COVID-19 transmission were unanswered at that time, such as transmission among children. Significant restrictions have been placed on the nation’s 52 million school-aged children, including school closures, 6-foot distancing requirements, and outdoor masking while distancing; however, only a few grants were dedicated to study these questions in this unique population, creating challenges for evidence-based policymaking.
America’s children are still victimized by masking and other measures schools and politicians impose on them, despite the lack of supporting data. The authors also suggest the deficit of research on fundamental questions, like how the virus spreads and when infected individuals are most contagious, led to the politicization of the response. “In the absence of evidence-based answers to the common questions the public was asking, political opinions filled that vacuum,” they wrote.
“The NIH, as the largest research-funding arm of the federal government, has a responsibility to fund research that can address misinformation with evidence,” the authors continued. “A resilient health care system in times of crisis should be able to pivot funding toward specific grants answering critical gaps in knowledge. NIH may consider developing procedures to rapidly pivot funding and guidelines for reviewing targeted proposals relevant to addressing a public health emergency.”
These findings demonstrate that our public health agencies are in serious need of reform. They have failed the people who fund them for the last two years. Clearly, the NIH is not agile or flexible enough to pivot to handling a health crisis, and there is ample reason to suspect a degree of institutional capture by Big Pharma. When Republicans hold majorities in Congress, they must reevaluate the NIH and other public health agencies’ funding, mission, and authority. Action is essential to restoring trust in public health before the next emergency.







Join the conversation as a VIP Member