There is new data that may explain how biological gender factors into the risk of severe illness related to COVID-19. In a retrospective study of those admitted to an ICU in Germany, it was found that the majority of male patients presented with low testosterone. This study was motived by both local and global data.
Men were being admitted to ICU with severe disease at a 3.5:1 ratio in the German hospital. The increased mortality and severe disease in men were noted globally as well. It was also consistent with the disease pattern in SARS and MERS. From NPR:
Sabra Klein, a researcher at the Johns Hopkins Center for Women’s Health, Sex, and Gender Differences, began noticing hints of a sex difference in COVID-19 infections back in February as reports began to emerge from China. She knew that an increased risk to men has been observed for other severe coronaviruses that have appeared in the past.
“What I was seeing was a pattern that held true in the SARS outbreak that occurred in Hong Kong,” she says, “as well as the ongoing MERS outbreak in the Middle East.”
The German study focused on sex hormones that play a specific role in the immune response. It looked at the clinical record and lab values of 45 patients admitted to the ICU who had died or been discharged between March 8, 2020, and April 29, 2020. The labs were drawn upon admission to eliminate the impact of any other COVID-19 treatment or therapeutic intervention.
All 35 men and 10 women evaluated had some preexisting condition. The most common was hypertension followed by cancer, obesity, type II diabetes, and heart disease. Each blood serum sample was tested for 12 hormones and 24 immune markers called cytokines and chemokines.
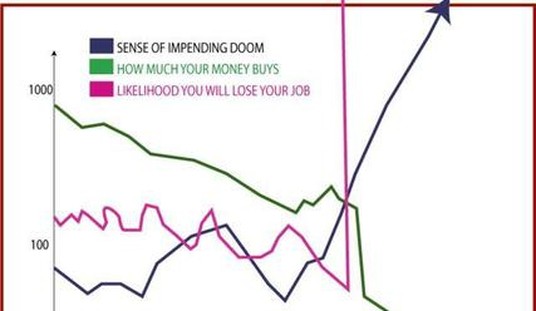
Because of other independent research suggesting that that severe COVID-19 illness may be linked to a cytokine storm, or a syndrome where a person’s immune system overreacts to an illness, the researched looked at how the levels of key hormones and the immune response varied in the patient population.
They found male hormones played a role in both men and women:
In general, low testosterone levels in male COVID-19 patients correlate with inflammatory cytokine expression. In contrast, high testosterone levels in female COVID-19 patients correlate with elevated expression of inflammatory cytokines. Thus, testosterone exerts a protective immune response in men, while accelerating inflammation in women.
Similar patterns and immune system responses were noted in the original SARS outbreak as well. According to an article in Nature in 2003 (emphasis mine):
The researchers aren’t just worried that SARS might make a comeback – although that is still a real possibility. They are concerned because it seems to have killed people by triggering a runaway release of inflammatory chemicals called cytokines, in a so-called “cytokine storm” that can be more deadly than the virus itself. This is how numerous diseases kill, from pneumonia to flu, making it one of the hottest topics in infectious disease research right now. And it has proved maddeningly hard to treat, with average fatality rates topping 50 per cent in full-blown “septic shock”, as the clinical condition is known.
SARS, a coronavirus that came from nowhere to kill around 1 in 6 of its victims, has added an urgent impetus to the research. There’s reason to believe that any new infectious disease that crosses from animals to humans could trigger this reaction. “A lot of people are clued into this as a very important way of understanding viruses,” says virologist Wendy Barclay at the University of Reading, UK. “It’s an up-and-coming subject.”
The study concludes that men with low levels of these gender-based hormones have a more difficult time generating an effective immune response:
However, analyzing major sex hormones, we found that the vast majority of male COVID-19 patients suffer from severe testosterone (68.6%) and dihydrotestosterone (48.6%) deficiencies upon hospital admission. Thus, it seems rather unlikely that patients with such a lack in key AR activating factors will be able to mount immune responses to combat viral infections.
This finding also aligned with findings during the avian flu outbreak:
This is in line with our findings here that low testosterone levels correlate with high levels of inflammatory cytokines. Moreover, in the avian H7N9 human cohort, low testosterone levels in male H7N9 patients strongly correlated with lethal
outcome.
Understanding the role of hormones related to an individual’s gender and how these can vary with other preexisting conditions may be part of unlocking a more specific risk profile for those at risk for severe illness. For example, increasing age, obesity, and diabetes can all affect testosterone production.
The immune system is a complex body system. Understanding the range of preexisting and genetic conditions that can impact its function may become the key to successful treatment. Dr. Thomas Yadegar at Providence Cedars-Sinai made clear that the protocols he was using to treat COVID-19 patients with what presented as a cytokine storm were individualized to a patient’s clinical presentation.
Because of the number of factors that can impact an individual’s immune response based on age, gender, and preexisting conditions, it is possible in viruses that cause this reaction there will not be a magic bullet. Rather, we need an entire arsenal based on a patient’s detailed clinical presentation. As it is highly likely we will see another animal-borne illness transfer to humans, there should be significant resources dedicated to mapping these factors and interventions out.
Editor’s Note: Want to support PJ Media so we can keep telling the truth about China and the virus they unleashed on the world? Join PJ Media VIP and use the promo code WUHAN to get 25% off your VIP membership.








Join the conversation as a VIP Member