Medicine, as it’s practiced in the United States, is defensive in nature. There’s a test or a treatment for everything, “just to be on the safe side.” While it’s reassuring for most of us to know that the cough and fever we have isn’t bubonic plague or pneumonia, it also causes healthcare costs to skyrocket and in a pandemic, vital resources are employed unnecessarily.
This appears to be what’s happening with ventilator machines. Intensive care doctors are now questioning the widespread use of ventilators.
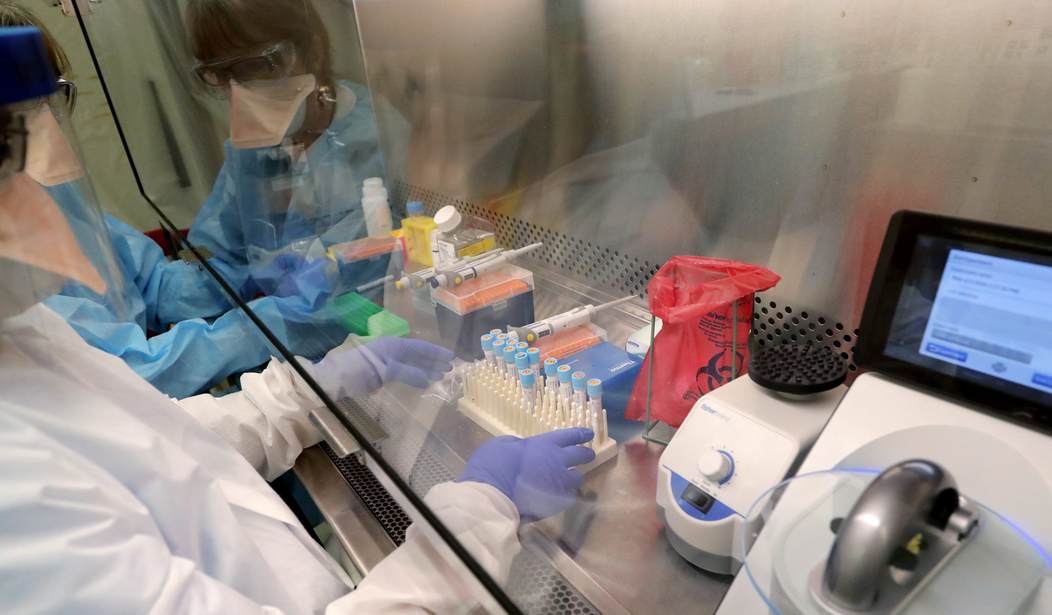
Even as hospitals and governors raise the alarm about a shortage of ventilators, some critical care physicians are questioning the widespread use of the breathing machines for Covid-19 patients, saying that large numbers of patients could instead be treated with less intensive respiratory support.
If the iconoclasts are right, putting coronavirus patients on ventilators could be of little benefit to many and even harmful to some.
Four months after the world first learned of the coronavirus (after it had been ravaging China for weeks) we still don’t have vital information about it that could help clinicians tailor treatments to get the maximum benefit from the resources expended.
What’s driving this reassessment is a baffling observation about Covid-19: Many patients have blood oxygen levels so low they should be dead. But they’re not gasping for air, their hearts aren’t racing, and their brains show no signs of blinking off from lack of oxygen.
This is extremely puzzling. Doctors have set treatments to deal with specific maladies and low blood oxygen levels are treated with some kind of mechanical assistance for breathing. The ventilators keep vital organs from failing. Besides, data from Chinese doctors suggest that the earlier you intubate a COVID-19 patient, the better chance they have. That’s the way it’s always been. So what’s different now?
That is making critical care physicians suspect that blood levels of oxygen, which for decades have driven decisions about breathing support for patients with pneumonia and acute respiratory distress, might be misleading them about how to care for those with Covid-19. In particular, more and more are concerned about the use of intubation and mechanical ventilators. They argue that more patients could receive simpler, noninvasive respiratory support, such as the breathing masks used in sleep apnea, at least to start with and maybe for the duration of the illness.
Now, all doctors have to do is figure out which patients don’t need ventilators despite their symptoms.
“I think we may indeed be able to support a subset of these patients” with less invasive breathing support, said Sohan Japa, an internal medicine physician at Boston’s Brigham and Women’s Hospital. “I think we have to be more nuanced about who we intubate.”
Speaking as someone who has been sedated for four days and had a ventilator tube rammed down his throat, if doctors can avoid using the procedure, they should. Perhaps as we learn more about the disease, doctors can better determine who actually needs a ventilator and when they need it, rather than reacting defensively and going immediately to mechanical breathing equipment, which is in short supply during this pandemic, at the first sign of trouble








Join the conversation as a VIP Member