The state of Georgia is preparing to offer a limited number of lower-income people Medicaid coverage in exchange for 80 hours of work or volunteering a month.
The Biden administration surprisingly decided not to appeal a federal court ruling that granted Georgia the right to try the work-for-Medicaid program — a program first approved during the Trump administration for 12 states but later canceled by Biden.
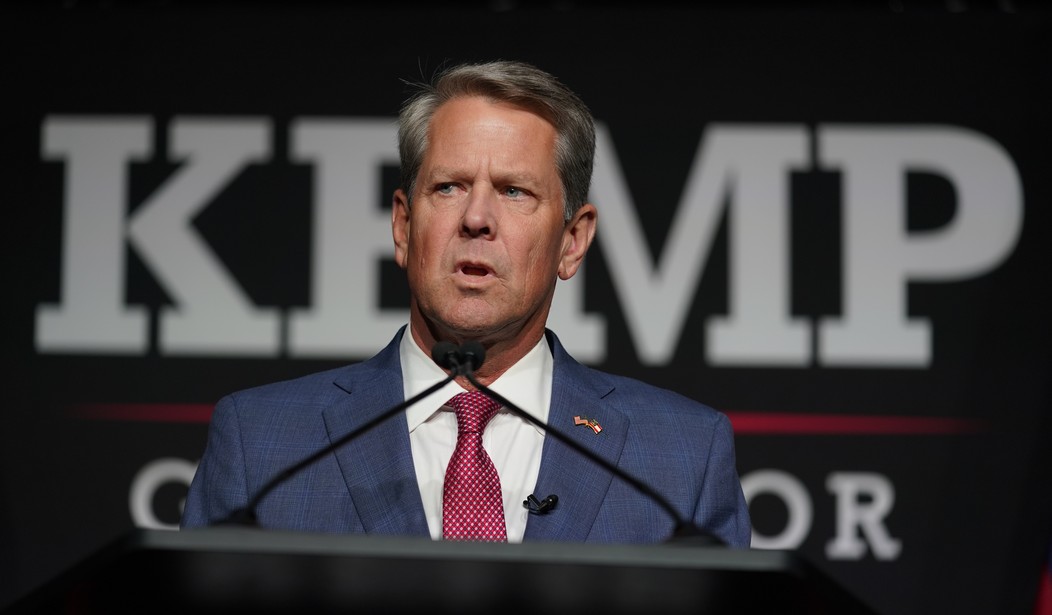
The program will actually cost significantly more than standard Medicaid coverage and the program’s strict requirements won’t cover a lot of Georgians. But Kemp believes it’s worth doing.
“The best-case scenario is that some uninsured Georgians would get coverage for some amount of time,’’ Laura Colbert, executive director of the consumer advocacy group Georgians for a Healthy Future, told the Atlanta-Journal Constitution. “It’s going to be a big headache for the state and for people who enroll or try to enroll.”
Georgia’s per-enrollee cost for the work requirement program is expected to be at least three times higher than it would be under a regular Medicaid expansion, said Colbert.
The federal government would have paid for at least 90% of the costs of insuring hundreds of thousands of Georgians under a full expansion. That compares with the expected 67% matching rate from the feds under the slimmer Kemp plan. And that difference doesn’t account for a Biden administration incentive for expansion that would net Georgia $710 million, according to a KFF estimate.
Indeed, barriers to enrollment will keep most poor Georgians off the rolls. “Full-time caregivers, people with mental health conditions or substance use disorders, and people unable to work but who have not yet qualified for disability coverage would find it hard to qualify,” reports the AJC.
The high cost and smaller number of potential participants raise the question of why not accept the full-blown Medicaid expansion offered under Obamacare. Most states that refused the full expansion at first, worried that Obamacare would be declared unconstitutional and repealed, have now accepted the reality of Obamacare’s existence and are moving to full expansion.
Related: How to Bring Social Security and Medicare Spending Under Control
Kemp’s idea of a “workfare” program is a good one. The “moral hazard” of getting something for nothing courtesy of the taxpayer needs to be addressed and this is certainly one way to do it.
But is it really the best way?
Many people struggling with homelessness in Georgia would likely not meet the work or volunteer thresholds, said Kathryn Lawler, CEO of Saint Joseph’s Health System, an Atlanta-based nonprofit.
Sixty percent of patients at its Mercy Care community health centers are homeless, she said. Coverage through Medicaid expansion would let patients afford health care, address chronic conditions, and relieve the stress of medical bills, she said.
People who need medical care often are too sick to go to work, Lawler said, adding that a single mother with three small children could be deemed ineligible. Full Medicaid expansion, through increased payments to providers, would ultimately allow Mercy Care to serve more people in need, she said.
The Biden administration didn’t appeal the original federal court decision that’s allowing the program to go forward. Some observers believe it may be waiting to see if the program fails or not. Others think that if it had taken the case to another appeals court, the judges may have affirmed its legality, thus strengthening the program.
Kemp says the program will go live in July.









Join the conversation as a VIP Member