Gilead Science has announced the pricing of remdesivir to treat the typical COVID-19 patient. Honestly, $3,210 is not bad for a drug that was developed years ago that didn’t work for the intended disease. Drug development is expensive, and those costs need to be recovered. The price will become effective in July after the manufacturer donated the treatment through May and June.
There will be a two-tiered pricing system in the United States with patients who are commercially insured paying more. How much more isn’t clear, but for those on Medicare, the cost will be $390 per dose. The pitch is that this will reduce the number of days a patient is in the hospital by an average of four. Gilead Chief Executive Daniel O’Day estimates an average of $12,000 in length-of-stay savings.
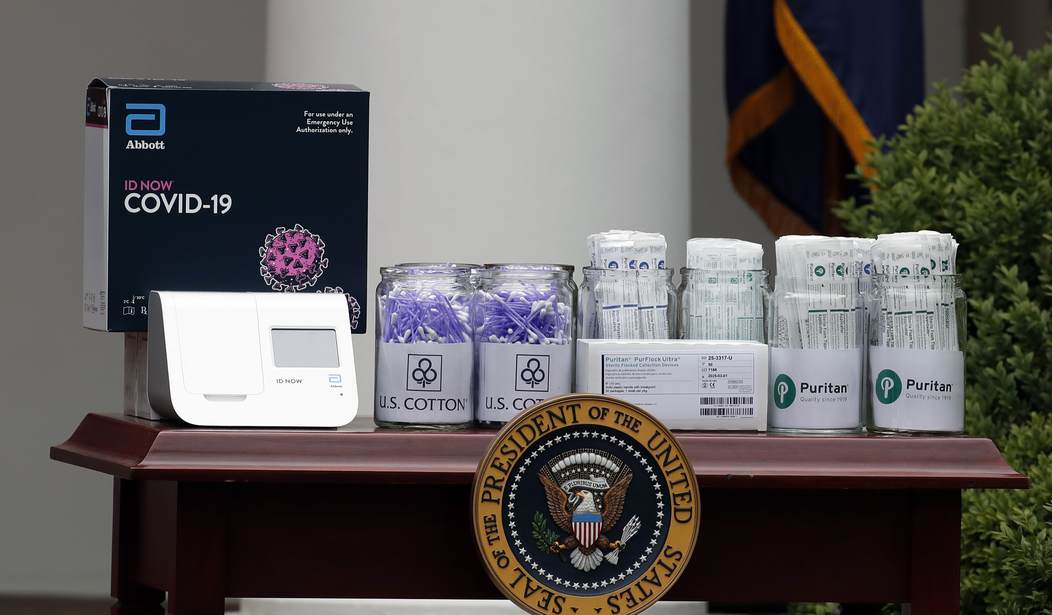
Remdesivir
According to the NIH, remdesivir shows statistically significant improvement for those requiring supplemental oxygen in days to recovery. According to the clinical trial, it does not improve mortality rates in a significant way. Stated differently, people who were going to get better, get better faster. Those who were not will still die.
So while it can improve recovery time, it does not do what we would hope. It does not save lives. However, doctors and researchers are providing what could be lifesaving treatments that are not getting nearly enough attention.
Cytokine Storms
The Wall Street Journal and several clinicians have reported that a significant number of patients who contract COVID-19 become severely ill with a condition called a cytokine storm. This syndrome is an overreaction of a patient’s immune system that can mimic an autoimmune disorder.
An autoimmune disorder causes a person’s immune system to attack other body tissues. This process would explain the full range of symptoms described in severe COVID-19 as well as the persistent damage to various body systems that extend beyond recovery from the virus.
Dr. Thomas Yadegar gave the best explanation of this syndrome and how to identify and treat it in April. He acknowledges that severe COVID-19 can take two paths. One is in compromised patients who develop severe viral pneumonia. The other is a cytokine storm that causes the autoimmune response.
Then, Dr. Yadegar had treated over two dozen patients using the treatment protocols for the cytokine storm, and none had died or required a ventilator. To provide the treatment, he used immunosuppressants and powerful steroids. While this seemed counterintuitive, it worked to solve the underlying problem causing the immune system dysfunction.
Clinical trials from the United Kingdom recently supported his approach. Researchers there demonstrated that dexamethasone, a potent corticosteroid, demonstrated lifesaving results. Unlike remdesivir, it showed a statistically significant reduction in deaths from COVID-19 for patients on ventilators and supplemental oxygen.
The logical follow-up to Dr. Yadegar’s work and the U.K. study is to determine the differential diagnosis between severe viral pneumonia and cytokine storms if one exists. It may be possible they occur together. The NIH acknowledges the incidence of cytokine storms, which result in sepsis or septic shock. In a post last updated May 18, 2020, they note:
The data so far available seem to indicate that the viral infection is capable of producing an excessive immune reaction in the host. In some cases, a reaction takes place which as a whole is labeled a ‘cytokine storm’. The effect is extensive tissue damage with dysfunctional coagulation.
If the NIH knows this, why don’t most Americans? It seems to be the origin of the most deadly and destructive forms of the disease. There is also hope to treat it using the drug classes discussed by U.K. researchers and Dr. Yadegar. These drugs cost a fraction of what remdesivir does.
Hydroxychloroquine
Another drug that costs a fraction of what remdesivir does is hydroxychloroquine. It is used in combination with azithromycin and zinc. This drug was highly politicized early in the pandemic because the president expressed hope that it could be effective.
At that time, doctors in the United States who were using the drug combination were clear. It should be used early in the infection, especially in those in high-risk groups. However, the emergency use authorization given by the FDA provided the drug to individuals suffering from severe disease. As discussed above, many of these patients are suffering from a complex, multi-system illness that requires more than a drug combination that slows viral replication.
However, Yale researcher Harvey Risch, M.D., Ph.D., has done a review of studies where the drug combination was used in an outpatient setting. Five studies, including two controlled clinical trials in process, convinced him to conclude in his abstract (emphasis mine):
Hydroxychloroquine+azithromycin has been used as standard-of-care in more than 300,000 older adults with multicomorbidities, with estimated proportion diagnosed with cardiac arrhythmias attributable to the medications 47/100,000 users, of which estimated mortality is <20%, 9/100,000 users, compared to the 10,000 Americans now dying each week. These medications need to be widely available and promoted immediately for physicians to prescribe.
His full study, published in the American Journal of Epidemiology, takes the nation’s health agencies and the media to task for overstating the risk for cardiac problems when using the drug combination. Dr. Risch’s calculations and the study results demonstrate that far more lives are saved and fewer hospitalizations are occurring when using it. The deaths arising from arrhythmias are very few.
He also makes a clear distinction between the two presentations of COVID-19. He states early treatment is focused on a viral replication problem that triggers the immune response seen in more severe cases. In an interview he said:
Interviewer: But the use of hydroxychloroquine to treat COVID-19 remains highly controversial. Why is there so much disagreement if it is effective?
Dr. Risch: I think that there has been confusion about treating the cold versus treating the pneumonia. These medications don’t seem to work so well for treating the pneumonia. As early as possible is crucial, within the first five to six days of symptoms.
As Dr. Risch notes:
The key to returning society toward normal functioning and to preventing huge loss, of life, especially among older individuals, people with comorbidities, African Americans and Hispanics and Latinos, is a safe, effective and proactive outpatient treatment that prevents ORIGINAL hospitalization in the first place.
Demand Answers
A potential solution to the problems presented by COVID-19 is a particularly good reason for the media to ignore his findings as well as not reporting Dr. Risch’s persuasive data-driven argument for using hydroxychloroquine in combination. That would allow everyone to go back to something near normal, and President Trump would be vindicated.
However, our national health agencies should have to answer the issues Dr. Risch raises regarding their failure to test in appropriate settings, the overstatement of risk, and the promotion of flawed studies like the one done at the VA.
These agencies are responsible for safeguarding the nation’s physical and emotional health. Ignoring the findings that Dr. Risch highlights is malpractice of the highest order. The next time Dr. Fauci in on television, someone should be brave enough to ask.








Join the conversation as a VIP Member