A trip to the emergency room is a scary, harrowing experience. But for too many Americans, even worse pain and suffering begin after the trip to the hospital is over and the healing has begun – when surprise medical bills come in the mail.
Surprise medical bills are charges slapped on insured patients when they inadvertently receive health care from an out-of-network provider. This can happen when an individual is traveling and doesn’t have access to an in-network provider, or is taken by ambulance to an emergency room not covered by their insurance network.
It can even happen when a patient receives care from an approved, in-network hospital, but an out-of-network doctor is brought in to provide care.
These quirks of insurance can result in devastating five- and six-figure medical bills.
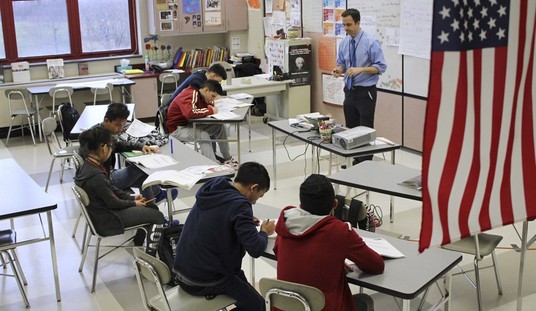
Drew Calver knows the disastrous impacts of a surprise medical bill all too well. EMTs rushed the Austin, Texas-area high school history teacher to the nearest emergency room in an effort to treat a near-fatal heart attack. In the hospital, Calver was told his insurance would cover the life-saving medical care. His insurer, however, later determined the hospital was out-of-network and slapped Calver with a $108,000 medical bill.
In Salt Lake City, Utah, Lisa Ray’s 16-year-old son broke his jaw playing rugby. The local in-network hospital was too full to accept him as a patient and sent the family to another hospital for emergency surgery. As a result of her son receiving treatment in the out-of-network hospital, Lisa was forced to pay more than $27,000 out of her own pocket.
Insurance companies, in an effort to pay as little as possible and shift costs to their customers, concoct narrow and confusing policies that make it difficult to avoid out-of-network expenses that result in surprise medical bills. As a result, paying for health insurance is becoming less appealing to many Americans.
From 2016 to 2018, unsubsidized health insurance enrollment fell by more than 2.5 million people – a drop of 40 percent.
Clearly, something has to be done to prevent these unreasonable charges for insured Americans and restore the public’s faith in health insurance. Regrettably, most of the plans Congress has come up with to address surprise medical bills do little to reduce costs to patients – and come with devastating side-effects to health care providers.
Proposals floating around Congress include socialist-style price controls that would short-change doctors, push qualified health care professionals out of the medical field, and limit choice for patients.
Two bills in the House of Representatives include a mediation process to determine a price when insurers and out-of-network providers can’t agree on a payment rate. From a distance, this arbitration sounds like a reasonable, market-based approach to reducing out-of-network expenses.
Unfortunately, the mediation process is a sham that forces the judge to follow a pricing structure developed by insurance companies. As a result, the only winner will be insurers. Patients will continue to get the shaft, and health care providers will receive artificially low payment rates for services, making it financially impossible for some doctors and hospitals to conduct business.
The best prescription for solving the surprise medical billing plague is for insurers to stop writing convoluted rules that make it difficult for well-meaning patients to stay in-network. Congress should step in and penalize insurance companies that represent medical facilities as being in-network when they aren’t. Similarly, hospitals should also be penalized when they tell patients they are in-network, but bring in out-of-network doctors to treat patients without the patients’ knowledge.
But for now, Congress doesn’t seem interested in such fair, common-sense policy reforms. Instead, lawmakers from both parties are focused on creating an unfair playing field where insurance companies continue to get richer, while patients and health care providers suffer.
Drew Johnson is a government watchdog who serves as a senior fellow at the National Center for Public Policy Research.






Join the conversation as a VIP Member