JULIE KELLY SAYS THE SOCIAL DISTANCING EXPERIMENT HAS FAILED:
“We expected that we would start seeing more significant declines in new cases and deaths around the nation at this point, and we’re just not seeing that.”
In fact, Gottlieb pointed to rising daily COVID-19 cases in 20 states, including heavily locked-down states such as Virginia and Maryland.
But this seems to defy the “science” that governors and lawmakers repeatedly pledge to follow in order to keep people safe from the virus.
After all, Virginia Governor Ralph Northam issued his first social distancing order on March 17 to “stop the spread of the virus in the Commonwealth,” as he promised. A few weeks later, Northam, a physician, joined Maryland Governor Larry Hogan and Washington, D.C. Mayor Muriel Bowser to announce a collective shelter-in-place decree after residents failed to obey their original commands.
“What we’re seeing now is the result of how people interacted two or three weeks ago,” Northam scolded on March 30. “What we will see a few weeks from now will be determined by how people behave today and in the following days.”
But five weeks later, the area is reporting a record number of COVID-19 cases. Yes, of course, testing is ramping up, too—but considering the harsh stay-at-home orders, how and why are people still getting infected?
It turns out, as I wrote last month, “social distancing” is untested pseudoscience particularly as it relates to halting the transmission of the SARS-CoV-2 virus. On its website, the CDC provides no links to any peer-reviewed social distancing studies that bolster its official guidance.
Well, to be fair, you only need double-blind studies when you’re assessing drugs that President Trump mentions favorably.
But seriously, the lockdowns were sold as, and were originally meant to be, stopgaps to ensure that the number of cases didn’t outrun healthcare capacity. That’s not an issue — not even in NYC, where they’re closing field hospitals for lack of patients — and that means it’s time to reopen.
Related: Sean Trende: Policy and Punditry Need to Adapt to New Virus Data.
When we began our foray into quarantine seven weeks ago, there was a unifying and eminently sensible rationale behind it: “Bend the curve.” The idea was this: If allowed to go unchecked, COVID-19 would overwhelm hospitals, leaving patients without beds. Short on ventilators, patients would be left to suffocate. In short, by slowing the spread of the virus we would prolong the amount of time it spread through the country, but would reduce the total number of deaths. Moreover, we would buy time for the nation’s testing apparatus to ramp up, to produce more ventilators, and to expand hospital capacity. . . .
If this really was the goal, then “job well done,” as they say, or at least largely so. . . . There are many interesting stories within these data, but the main takeaway should be relatively clear: No states are on anything resembling an exponential growth trajectory, almost all states are past a peak, and most states are substantially so. This would suggest that in many states, the question really should be how to reopen while keeping hospitals from being overwhelmed again.
This is especially true given that the situation on the ground has changed dramatically since early March. Most states have substantially expanded hospital capacity, both by securing emergency locations to be used in case of overflow and by suspending elective surgeries, to the point where many hospitals are facing financial crises. Moreover, the arrival of the first COVID-19 therapeutic, Remdesivir, will help, since hospital stays are shortened when the drug is used. Personal protective equipment and ventilator availability has expanded, we’ve developed techniques for sanitizing PPEs, and ventilators may not be as useful as once thought. As of this writing, we’re testing over 200,000 people a day, which eclipses the rate South Korea achieved when containing its viral outbreak.
Perhaps most promisingly, the death rate looks lower than initially expected. It isn’t clear how much lower – studies disagree – but most of the serological studies find an implied fatality rate lower than the 1% used to arrive at the conclusion that 2 million people would die if the virus were allowed to run its course. Likewise – this is much less commented upon although it might be more important – the hospitalization rate looks substantially lower than initially anticipated.
Read the whole thing. We hear a lot about science. Science means changing your understanding based on the data.
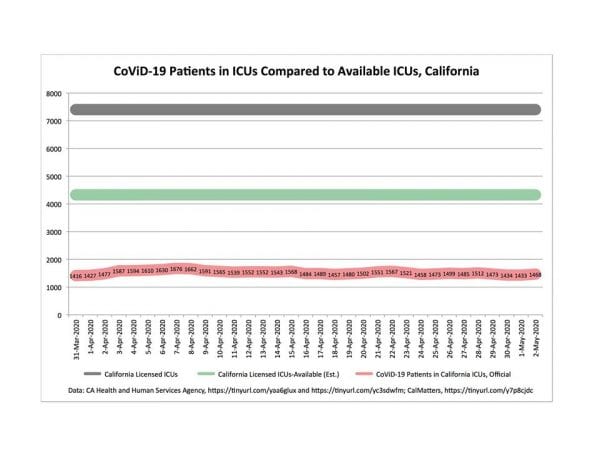
And speaking of success at bending the curve here’s a chart prepared by Chapman U. lawprof Tom W. Bell showing how little pressure there is on California ICU beds: